A nurse is discussing comorbidities associated with eating disorders, an intricate interplay of physical, mental, and metabolic conditions that often accompany these complex mental health challenges. This article delves into the prevalence, impact, and management of these comorbidities, offering insights into the multifaceted nature of eating disorders and their implications for patient care.
The prevalence of cardiovascular issues, gastrointestinal complications, and bone health concerns among individuals with eating disorders highlights the significant physical toll these conditions can take. Mental health comorbidities, such as depression, anxiety, and obsessive-compulsive disorder, further compound the challenges faced by these individuals.
1. Physical Comorbidities: A Nurse Is Discussing Comorbidities Associated With Eating Disorders
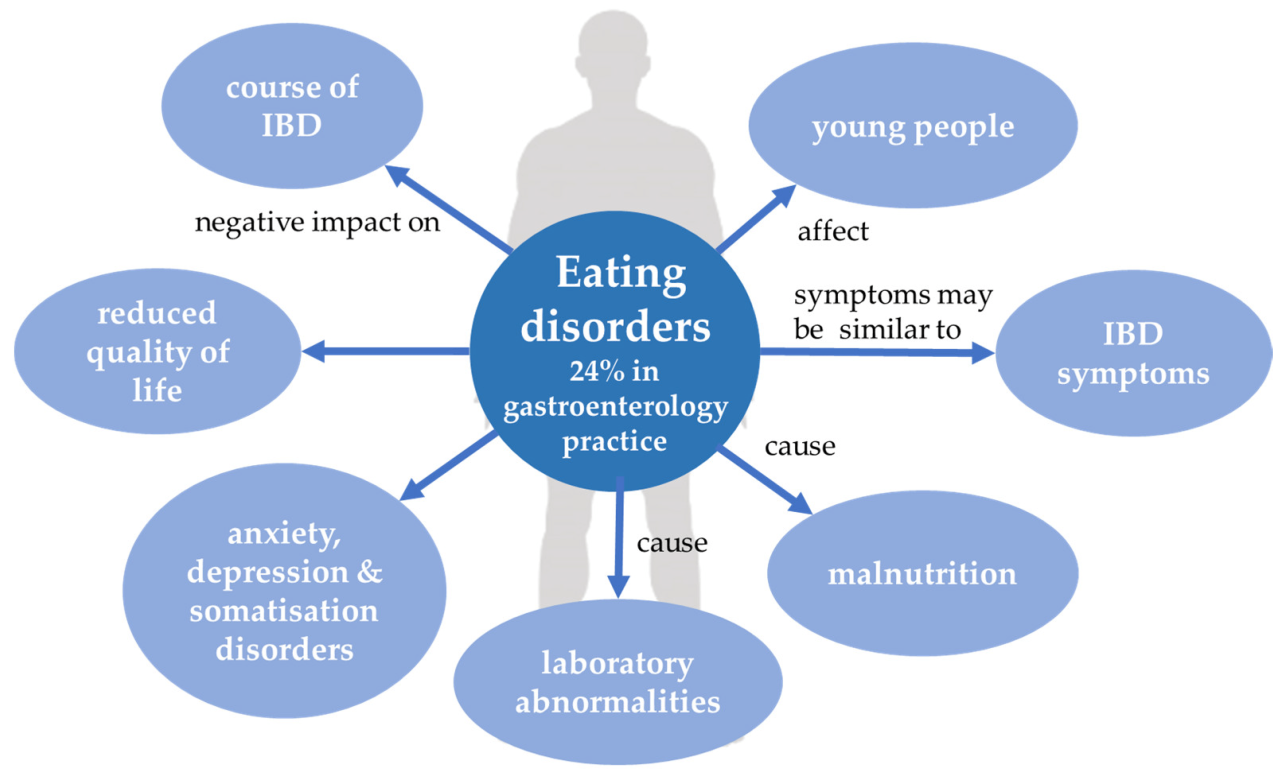
Eating disorders are associated with a range of physical comorbidities, including cardiovascular issues, gastrointestinal complications, and malnutrition-related problems.
Cardiovascular Issues
Individuals with eating disorders have an increased risk of cardiovascular issues, such as heart rhythm disturbances, coronary artery disease, and sudden cardiac death. This is primarily due to the malnutrition and electrolyte imbalances that often accompany these disorders.
Gastrointestinal Complications, A nurse is discussing comorbidities associated with eating disorders
Eating disorders can also lead to gastrointestinal complications, such as gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), and pancreatitis. These complications can result from the disordered eating patterns, purging behaviors, and malnutrition associated with eating disorders.
Malnutrition-Related Problems
Malnutrition is a common consequence of eating disorders and can have a significant impact on bone health and muscle mass. Osteoporosis, a condition in which bones become weak and brittle, is common among individuals with eating disorders. Muscle wasting, or sarcopenia, is another common complication that can lead to weakness and impaired physical function.
2. Mental Health Comorbidities
Eating disorders are often comorbid with mental health conditions, such as depression, anxiety disorders, obsessive-compulsive disorder (OCD), and substance use disorders.
Depression and Anxiety Disorders
Depression and anxiety disorders are the most common mental health comorbidities associated with eating disorders. These conditions can contribute to the development and maintenance of eating disorders and vice versa.
Obsessive-Compulsive Disorder (OCD)
Eating disorders can exacerbate OCD symptoms, such as intrusive thoughts, compulsive behaviors, and perfectionism. This is because eating disorders and OCD share similar neurobiological mechanisms, including alterations in serotonin and dopamine pathways.
Substance Use Disorders
Substance use disorders are also common among individuals with eating disorders. This is because both conditions involve impulsive behaviors and attempts to regulate mood and emotions.
3. Metabolic Comorbidities
Eating disorders can also lead to metabolic comorbidities, such as metabolic syndrome, hormonal imbalances, and thyroid dysfunction.
Metabolic Syndrome
Metabolic syndrome is a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. It is characterized by high blood pressure, high blood sugar, excess body fat around the waist, and low levels of “good” cholesterol.
Eating disorders can increase the risk of metabolic syndrome due to malnutrition, weight fluctuations, and disordered eating patterns.
Hormonal Imbalances
Eating disorders can disrupt the body’s hormonal balance, which can lead to menstrual irregularities, infertility, and other health problems. For example, anorexia nervosa can cause amenorrhea, or the absence of menstrual periods.
Thyroid Dysfunction
Eating disorders can also affect thyroid function. Hypothyroidism, or an underactive thyroid, is common among individuals with eating disorders. This can lead to fatigue, weight gain, and other health problems.
4. Risk Factors and Protective Factors
There are several modifiable risk factors for developing comorbidities associated with eating disorders, including:
- Genetic predisposition
- Family history of eating disorders
- History of trauma or abuse
- Low self-esteem
- Body dissatisfaction
- Perfectionism
Protective factors that can reduce the risk of developing comorbidities include:
- Healthy coping mechanisms
- Strong social support
- Access to mental health treatment
- Early intervention and treatment for eating disorders
5. Treatment Considerations

Treatment for eating disorders and their comorbidities requires a multidisciplinary approach that involves medical, nutritional, and psychological interventions.
- Medical interventions may include monitoring vital signs, electrolyte replacement, and medication management.
- Nutritional counseling is essential for restoring a healthy diet and weight.
- Psychotherapy, such as cognitive-behavioral therapy (CBT), can help individuals address the underlying psychological issues that contribute to their eating disorder.
- Medication, such as antidepressants and anti-anxiety medications, may be used to manage comorbid mental health conditions.
Questions Often Asked
What are the most common physical comorbidities associated with eating disorders?
Cardiovascular issues, gastrointestinal complications, and bone health concerns are among the most prevalent physical comorbidities.
How do eating disorders impact mental health?
Eating disorders are often accompanied by mental health comorbidities, including depression, anxiety, and obsessive-compulsive disorder.
What is the role of nurses in managing comorbidities associated with eating disorders?
Nurses play a crucial role in early detection, intervention, and management of comorbidities, working within a multidisciplinary team to provide comprehensive patient care.